The Problem
Dr. Fungai Kavenga, MOHCC, highlighted the urgent need for such innovation,“Zimbabwe is struggling with a huge case detection gap, missing about 40%of the estimated TB cases as they go undiagnosed”. Infrastructural challenges such as the lack of electricity, reliable internet and equipment portability is also hinders efficiency of medical teams out in the field, putting a limit to the number of people that can be screened at any given time.
Short Read
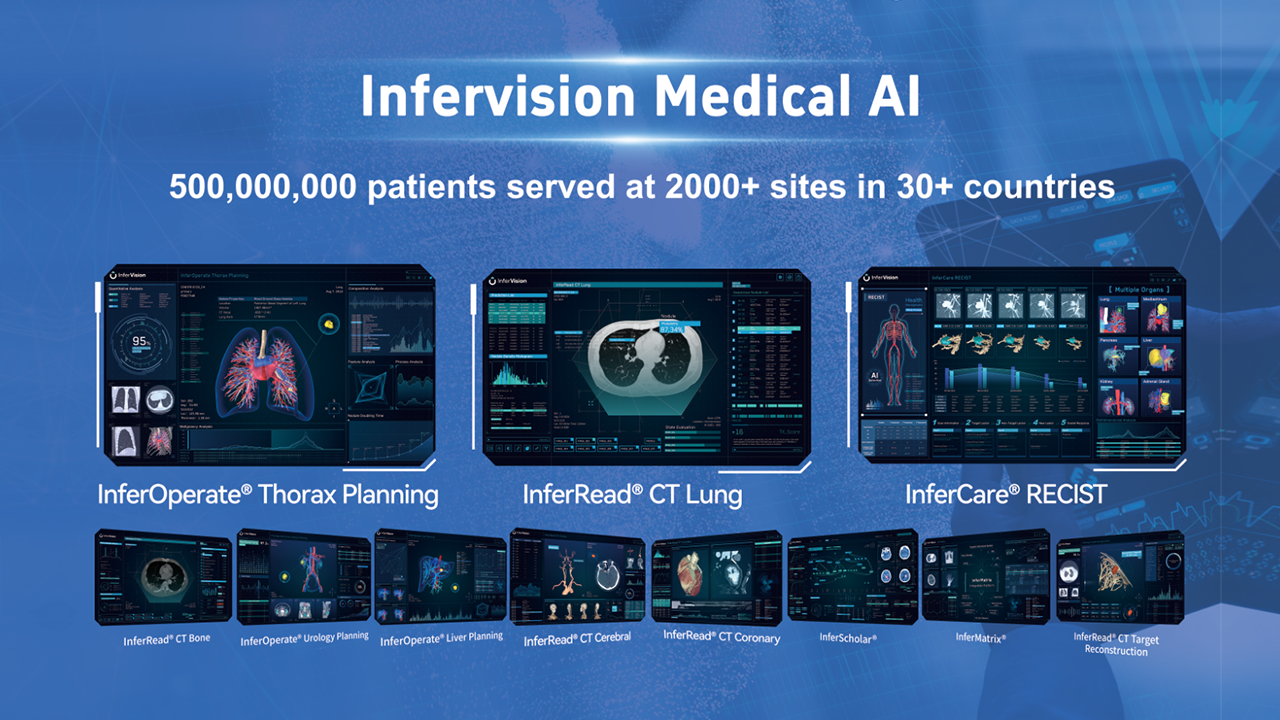
In 2021, tuberculosis (TB) was the leading cause of death in Zimbabwe, with over 14,000 undiagnosed cases. To address this, Zimbabwe's Ministry of Health and Child Care (MOHCC) partnered with Infervision to deploy InferAir, an AI-powered, ultra-portable X-ray solution. InferAir's lightweight design and offline capabilities make it ideal for remote areas with limited resources. Currently, over 2,600 people in rural Zimbabwe are being screened daily using InferRead and InferAir, significantly improving TB detection rates. InferAir can empower clinicians with rapid interpretation and offer evidence-based recommendations, improving efficiency and accuracy. Plans are underway to scale up its use nationwide. This case study demonstrates the successful implementation of AI and portable X-ray technology in combating TB in a resource-limited setting.

Combating TB in Rural Zimbabwe
.jpeg)
InferAir combines two game-changing advancements in TB screening technology – AI-powered computer-aided detection (CAD) , InferRead, and ultra-portable chestX-ray, designed for deployment in remote regions and resource-limited settings. Since2024, Infervision has collaborated with theMOHCC and international partners, including the Global Fund and United Nations Development Programme (UNDP), to launch alarge-scale screening project in Gweru, aremote district in Zimbabwe.

Over 10,000 additional cases will have been screened and detected by the end of 2024, saving many lives in Zimbabwe.
How it works
.jpeg)
Weighing just 25kg, a fraction of that of traditional X-ray equipment, InferAir can accurately screen up to 250 people for TB per day, while operating without access to internet or electricity- a crucial challenge in rural Zimbabwe. InferAir is designed to be efficient, with the chest X-ray images taken automatically interpreted by AI to provide a comprehensive analysis within 10 seconds, indicating whether someone should receive further diagnostic testing for TB. Detection stations can be set up quickly and easily, with the machines taking less than 5 minutes to be ready, and data can be stored locally or on the cloud once there is an active Internet connection.
What's Next
Infervision is currently working with the MOHCC to train a cohort of ‘superusers’ who will able to train subsequent batches of medical professionals to expand the capabilities of TB detection countrywide. Detection stations can be set up quickly and easily, with the machines taking less than 5 minutes to be ready, and data can be stored locally or on the cloud once there is an active Internet connection.
Testimonials

“It’s so easy to set up, we can get it going within 5 minutes, which means we can improve our efficiency in the number of cases we can screen per day.”

“I’m most excited about the aspect of quality control. Now we can check on how we interpret the X-rays, it’s like having a second opinion by your side in real time.”
Bringing TB detection and timely treatment, despite infrastructural challenges, to rural Zimbabwe is only the first step in turning the tide in the battle to end TB.
👆Click here to download the full case study!