OVERVIEW
In an exceptional demonstration of modern thoracic surgery, a team at The First Affiliated Hospital of Soochow University successfully performed a uniportal video-assisted thoracoscopic lobectomy (UVATS) on a patient with situs inversus totalis (SIT).
SIT is an autosomal recessive genetic condition in which the thoracic and abdominal organs are arranged as a mirror image of their usual configuration. The patient, diagnosed with lung adenocarcinoma, presented a unique set of challenges due to her reversed anatomy, which required precise preoperative planning and surgical expertise.

PATIENT PROFILE
- A 57-year-old non-smoking woman who sought medical attention for a persistent cough.
- A CT scan revealed a 35 × 25 mm tumor in the left middle lobe of her lung, with an additional 5-mm nodule in the upper lobe.
- Diagnosed with SIT, the patient’s reversed organ arrangement required careful evaluation and imaging.
- The confirmed diagnosis was adenocarcinoma, staged at cT2aN0M0 (stage IB).
- Her general health was stable, and no evidence of lymph node involvement or distant metastasis was found on PET/CT imaging.


3D RECONSTRUCTION
The team’s approach included a thorough preoperative workup and the use of advanced imaging techniques to ensure an accurate understanding of the patient’s reversed pulmonary and vascular anatomy.
Given the complexity posed by SIT, which includes the potential for unexpected vascular and bronchial variations, the surgeons opted for the UVATS approach.
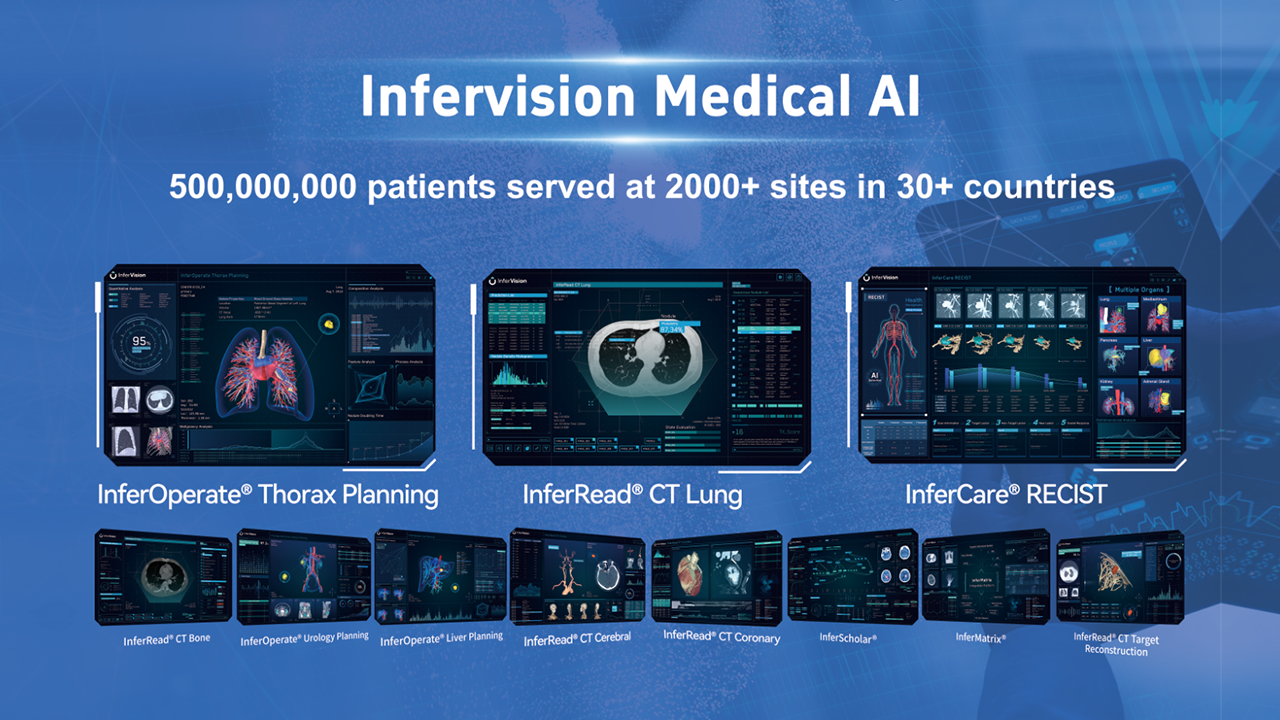
This choice was guided by the availability of Infervisions’s InferOperate 3D Thorax software, enabling precise anatomical mapping.
The 3D software confirmed that the left lung was structured into three lobes, separated by a well defined oblique fissure and a horizontal fissure, which was critical for planning the surgical approach.
Additionally, it allowed the surgeons to accurately anticipate the position of key structures like the azygos vein and superior vena cava, confirming their mirror-image arrangement, while noting the absence of the aortic arch in the left thoracic cavity.
With this detailed anatomical map, the team was able to locate the 3.0 cm tumor in the middle lobe with pleural depression and a 7 mm nodule in the upper lobe. This preoperative clarity guided their approach, helping them determine the safest incision site and ensuring precise, sequential excision of the middle lobe’s pulmonary veins, bronchus, and pulmonary artery branches.


SURGICAL PROCEDURE
The patient was positioned in the right lateral decubitus position, and general anesthesia was induced with one-lung ventilation using a double-lumen endotracheal tube (DLT).
The UVATS procedure commenced through a single 3-cm incision in the fourth intercostal space. Despite the reversed anatomy, the team successfully navigated the lung structures based on preoperative imaging. The left middle lobe and an upper lobe nodule were resected with minimal blood loss.
The patient was discharged without complications on the fourth day.
Histological analysis confirmed adenocarcinoma in the left middle lobe and chronic inflammation in the upper lobe nodule, with no carcinoma found in the surgical margins or lymph nodes.

CONCLUSION
This case underscores the significance of InferOperate 3D in handling complex anatomical variations. The surgical team’s expertise, combined with meticulous preoperative planning, facilitated a successful outcome in a challenging SIT patient.
No complications or recurrence were observed during the two-year postoperative period, illustrating that with the right tools and preparation, UVATS can be safely and effectively performed even in patients with rare congenital conditions like SIT.
Ready to transform your surgical planning?
👆Contact us today to schedule a demo with one of our team!
👆Click here to download the full case of the week!